
Common injuries that massage therapists see in their practice
Click on the injury to go directly to the section.
TORTICOLLIS
Massage therapy can be an effective treatment for neck pain.
Massage can help to:
- Relax tense muscles:
Massage can help to relax the muscles in the neck, which can reduce muscle spasms and tension headaches. - Improve circulation:
Massage can help to improve blood flow to the neck, which can help to reduce inflammation and promote healing. - Enhance mobility:
Massage can help to improve range of motion in the neck, which can help to reduce pain and stiffness. - Reduce stress:
Massage can help to reduce stress and promote relaxation, which can have a positive impact on neck pain.
It is important to note that massage may not be appropriate for all individuals with neck pain. A massage therapist working with a client with neck pain may use a variety of techniques to address the client’s specific needs and preferences. Some common techniques that may be used to address neck pain include:
- Swedish massage: This type of massage involves long, smooth strokes and kneading to help relax the muscles and improve circulation.
- Deep tissue massage: This type of massage involves the use of firm pressure and targeted strokes to reach deeper layers of muscle tissue. It may be helpful for releasing muscle tension and stiffness in the neck.
- Trigger point therapy: This type of massage involves the use of pressure on specific points in the muscles to help relieve muscle tension and pain.
- Myofascial release: This type of massage involves the use of gentle stretches and pressure to help release tightness in the fascia (connective tissue surrounding the muscles).
The pressure that is most appropriate for a client with neck pain will depend on the individual’s pain tolerance and specific needs. It is important for the therapist to communicate with the client to ensure that the pressure is comfortable and not causing any additional discomfort.
The therapist may also assess the muscles in the neck and surrounding areas to identify any areas of tension or dysfunction. Working on these muscles may help to relieve neck pain and improve mobility.
It is important to note that the specific techniques used and the approach taken will depend on the individual client’s needs and preferences, as well as the therapist’s expertise and training. It is always best for the therapist to work with the client to develop a treatment plan that is tailored to the client’s specific needs.
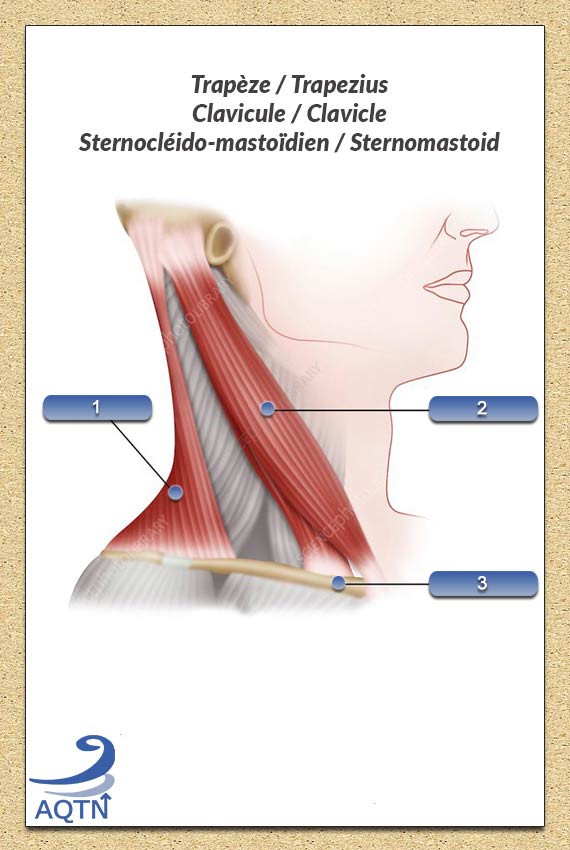
These are just a few examples of the muscles in the neck. There are many other muscles in the neck that contribute to movement and support of the head and neck.
There are several muscles in the neck that are responsible for movement and support of the head and neck. Some of the main muscles in the neck include:
- Sternocleidomastoid: This muscle runs from the sternum (breastbone) and clavicle (collarbone) to the mastoid process (a bony prominence on the skull) and is responsible for rotation and flexion of the head and neck.
- Scalenes: There are three scalene muscles in the neck (anterior, middle, and posterior) that run from the cervical vertebrae (bones of the neck) to the first rib. These muscles help to elevate and rotate the first rib during breathing and also assist with head and neck movement.
- Splenius: There are two splenius muscles in the neck (capitis and cervicis) that run from the midline of the spine to the base of the skull and the upper cervical vertebrae, respectively. These muscles help to extend and rotate the head and neck.
- Levator scapulae: This muscle runs from the transverse processes (projections on the sides of the vertebrae) of the cervical and upper thoracic vertebrae (mid-back) to the scapula (shoulder blade) and is responsible for elevating the scapula and rotating the neck.
- Trapezius: This large, triangular muscle extends from the base of the skull to the midline of the thoracic spine (upper back) and is responsible for extending, rotating, and elevating the head and neck, as well as moving the scapula.
Torticollis stretches
There are several stretches that may be helpful for someone with neck pain. It is important to consult with a healthcare professional or a trained therapist before starting any new stretching program, as certain stretches may not be appropriate for all individuals or may need to be modified depending on the individual’s specific needs and limitations.
Here are a few examples of stretches that may be helpful for neck pain:
- Neck tilt stretch:
Sit or stand upright with good posture. Slowly tilt your head to one side, bringing your ear towards your shoulder. Hold the stretch for 15-30 seconds, then slowly return to the starting position. Repeat on the other side. - Neck rotation stretch:
Sit or stand upright with good posture. Slowly turn your head to one side, bringing your chin towards your shoulder. Hold the stretch for 15-30 seconds, then slowly return to the starting position. Repeat on the other side. - Neck extension stretch:
Stand upright with good posture. Slowly tilt your head back, looking up towards the ceiling. Hold the stretch for 15-30 seconds, then slowly return to the starting position. - Neck flexion stretch:
Stand upright with good posture. Slowly bring your chin towards your chest, rounding your upper back. Hold the stretch for 15-30 seconds, then slowly return to the starting position
TIGHT OR INJURED TRAPEZIUS
There are several techniques and tools that may be helpful for releasing tension in the trapezius muscle using massage or manual therapy techniques.
Here are a few examples:
- Massage: Massage techniques such as Swedish massage, deep tissue massage, and trigger point therapy can be helpful for releasing tension in the trapezius muscle. The therapist may use a variety of strokes, such as kneading, petrissage, and effleurage, to help relax the muscle and improve circulation, also percussions if the condition allows for it.
- Myofascial release: Myofascial release techniques involve the use of gentle stretches and pressure to help release tightness in the fascia (connective tissue surrounding the muscles). These techniques may be helpful for releasing tension in the trapezius muscle.
- Foam rolling or tennis ball: Using a foam roller to apply pressure to the trapezius muscle can help to release tension and improve mobility.
- Heat therapy: Applying heat to the trapezius muscle, such as with a heat pack, can help to relax the muscle and reduce pain.
- Stretching: Stretching exercises that target the trapezius muscle, such as neck tilts, neck rotations, and neck extensions, can help to improve mobility and reduce tension in the muscle.
The origin of the trapezius muscle refers to the attachment point of the muscle on a stationary bone or structure. The origin of the trapezius muscle includes:
- The base of the skull: The trapezius muscle originates from the external occipital protuberance (a bony prominence at the base of the skull), the nuchal ligament (a band of connective tissue that runs along the base of the skull), and the spinous processes (projections on the posterior side of the vertebrae) of the seventh cervical vertebra (C7) and the T1-T12 thoracic vertebrae (mid-back).
- The clavicle (collarbone): The trapezius muscle also originates from the lateral (outer) third of the clavicle.
The insertion of the trapezius muscle refers to the attachment point of the muscle on a moveable bone or structure. The insertion of the trapezius muscle includes:
- The scapula: The trapezius muscle inserts into the superior (top) and medial (inner) borders of the scapula.
It is important to note that the trapezius muscle has three main regions: the superior (upper) region, the middle region, and the inferior (lower) region. Each region has its own specific actions and attachment points. It is also worth noting that the muscle may have additional attachment points or variations in structure in some individuals.
It is important to note that the specific techniques and tools used will depend on the individual’s needs and preferences, as well as the therapist’s expertise and training. The trapezius muscles is a large, triangular muscle divided in 3 parts, that extends from the base of the skull to the midline of the thoracic spine (upper back). It is responsible for extending, rotating, and elevating the head and neck, as well as moving the scapula (shoulder blade).
Stretches for trapezius
There are several stretches that may be helpful for releasing tension in the trapezius muscle. It is important to consult with a healthcare professional or a trained therapist before starting any new stretching program, as certain stretches may not be appropriate for all individuals or may need to be modified depending on the individual’s specific needs and limitations.
Here are a few examples of stretches that may be helpful for the trapezius muscle:
- Neck tilt stretch: Sit or stand upright with good posture. Slowly tilt your head to one side, bringing your ear towards your shoulder. Hold the stretch for 15-30 seconds, then slowly return to the starting position. Repeat on the other side.
- Neck rotation stretch: Sit or stand upright with good posture. Slowly turn your head to one side, bringing your chin towards your shoulder. Hold the stretch for 15-30 seconds, then slowly return to the starting position. Repeat on the other side.
- Neck extension stretch: Stand upright with good posture. Slowly tilt your head back, looking up towards the ceiling. Hold the stretch for 15-30 seconds, then slowly return to the starting position.
- Neck flexion stretch: Stand upright with good posture. Slowly bring your chin towards your chest, rounding your upper back. Hold the stretch for 15-30 seconds, then slowly return to the starting position.
- Shoulder blade squeeze: Stand upright with good posture. Squeeze your shoulder blades together and hold for 5-10 seconds. Relax and repeat.
ROTATOR CUFF INJURIES
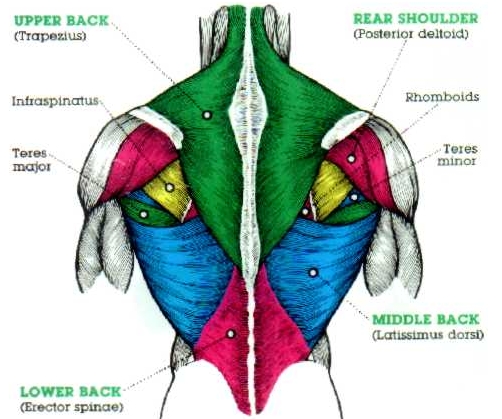
The rotator cuff is a group of four muscles and their corresponding tendons that attach the shoulder blade (scapula) to the upper arm bone (humerus). These muscles and tendons help to rotate and lift the arm. Massaging the rotator cuff muscles can be helpful for releasing tension and improving mobility in the shoulder. The rotator cuff is a group of four muscles and their corresponding tendons that attach the shoulder blade (scapula) to the upper arm bone (humerus). These muscles and tendons help to rotate and lift the arm. The insertion of the rotator cuff muscles refers to the attachment point of the muscle on a moveable bone or structure. The insertion points of the rotator cuff muscles include:
- Supraspinatus: This muscle inserts into the greater tubercle (a projection on the upper part of the humerus).
- Infraspinatus: This muscle inserts into the greater tubercle, near the posterior border of the humerus.
- Teres minor: This muscle inserts into the greater tubercle, near the posterior border of the humerus.
The origin of the rotator cuff muscles refers to the attachment point of the muscle on a stationary bone or structure. The origin points of the rotator cuff muscles include:
- Supraspinatus: This muscle originates from the supraspinatus fossa (a depression on the upper surface of the scapula) and the suprascapular ligament (a band of connective tissue that runs along the upper border of the scapula).
- Infraspinatus: This muscle originates from the infraspinatus fossa (a depression on the posterior surface of the scapula) and the suprascapular ligament.
- Teres minor: This muscle originates from the posterior border of the scapula, near the infraspinatus fossa.
- Subscapularis: This muscle originates from the subscapular fossa (a depression on the anterior surface of the scapula).
Here are some general guidelines for massaging the rotator cuff muscles:
- Use a variety of strokes: A combination of Swedish massage strokes, such as effleurage (light, sweeping strokes) and petrissage (kneading), and deep tissue techniques, such as cross-fiber friction and trigger point therapy, can be effective for massaging the rotator cuff muscles.
- Focus on the muscle attachments: Pay particular attention to the points where the rotator cuff muscles attach to the scapula and humerus, as these areas tend to be common sources of tension.
- Use your thumbs: The rotator cuff muscles are small and located deep within the shoulder joint, so it may be helpful to use your thumbs or elbow to apply pressure.
- Avoid direct pressure on the joint: Be careful to avoid applying direct pressure on the shoulder joint itself, as this can be painful and potentially harmful. Instead, focus on massaging the muscles surrounding the joint.
- Communicate with the client: As with any massage, it is important to communicate with the client to ensure that the pressure is comfortable and not causing any additional discomfort.
There are several stretches that may be helpful for relieving tension and improving mobility in the rotator cuff muscles. It is important to consult with a healthcare professional or a trained therapist before starting any new stretching program, as certain stretches may not be appropriate for all individuals or may need to be modified depending on the individual’s specific needs and limitations.
Scapular retraction stretch:
The scapular retraction stretch is a stretch that targets the muscles of the rotator cuff, as well as the muscles of the upper back and shoulders. This stretch is designed to help improve mobility and stability in the scapula (shoulder blade) and may also be helpful for relieving tension in the rotator cuff muscles.
To perform the scapular retraction stretch:
- Stand with your arms by your sides and your feet shoulder-width apart.
- Engage your shoulder blades by squeezing them together.
- Lift your arms straight out to the sides, keeping your elbows straight.
- Hold this position for a few seconds, then release.
- Repeat the stretch for a total of 10-15 repetitions.
Here are a few examples of stretches that may be helpful for the rotator cuff:
- Doorway stretch: Stand in an open doorway with your arms extended at shoulder height, palms facing forward. Slowly move your arms upwards until you feel a stretch in your shoulders. Hold for 15-30 seconds, then release.
- Cross-body stretch: Stand with your arms by your sides. Reach your right arm across your body and grab your left elbow with your right hand. Gently pull your left elbow towards your right shoulder until you feel a stretch in your left shoulder. Hold for 15-30 seconds, then release. Repeat on the other side.
- Towel stretch: Sit on a stable chair or bench with a towel wrapped around your hand. Hold the ends of the towel with your arms extended in front of you at shoulder height. Gently pull the towel towards your body until you feel a stretch in your shoulders. Hold for 15-30 seconds, then release.
- Wall stretch: Stand facing a wall with your arms extended in front of you at shoulder height, palms pressed against the wall. Slowly move your arms upwards until you feel a stretch in your shoulders. Hold for 15-30 seconds, then release.
It is important to keep good posture while performing this stretch, with your chest lifted and your shoulders relaxed. It is also important to start with a gentle stretch and gradually increase the intensity as you become more comfortable. As with any stretch, it is important to listen to your body and stop if you feel any pain or discomfort.
TENDONITIS
Tendonitis is an inflammation of a tendon, which is a strong, fibrous cord that connects muscle to bone. Tendonitis can occur when a tendon becomes overworked or strained, leading to irritation and swelling. Tendonitis can be caused by a variety of factors, including overuse, improper technique or posture, and poor conditioning.
Tendonitis can occur in any part of the body where there are tendons, but it is most common in the shoulders, elbows, wrists, knees, and ankles. Symptoms of tendonitis may include pain, swelling, stiffness, and difficulty moving the affected joint.
Treatment for tendonitis may include rest, ice, physical therapy, and medications to reduce inflammation and pain. In severe cases, surgery may be necessary to repair the damaged tendon. It is important to seek medical attention if you are experiencing symptoms of tendonitis, as untreated tendonitis can lead to further damage and disability.
A massage therapist may use a variety of techniques to help reduce inflammation and pain associated with tendonitis. These may include:
- Swedish massage strokes: Light, gentle strokes such as effleurage (sweeping) and petrissage (kneading) can help to increase circulation and reduce muscle tension.
- Deep tissue techniques: Techniques such as cross-fiber friction and trigger point therapy can be used to release muscle knots and break up scar tissue, which may be contributing to the inflammation.
- Stretching: Gentle stretches can help to improve range of motion and flexibility in the affected joint, which may help to reduce the strain on the tendon.
- Myofascial release: This technique involves applying gentle, sustained pressure to the tissues surrounding the muscle to release tension and improve mobility.
- Heat therapy: Applying heat to the affected area can help to increase blood flow and reduce muscle spasms and stiffness.
It is important to remember that every individual is different and may respond differently to treatment. It is best to consult with a healthcare professional or trained therapist for personalized recommendations on how to best manage tendonitis. Tendonitis can occur in any part of the body where there are tendons, but it is most commonly seen in the following muscles and tendons:
- Shoulder: The rotator cuff muscles (supraspinatus, infraspinatus, teres minor, and subscapularis) and the biceps tendon are common sites for tendonitis in the shoulder.
- Elbow: Tennis elbow (lateral epicondylitis) and golfer’s elbow (medial epicondylitis) are both forms of tendonitis that affect the elbow.
- Wrist: The wrist extensor muscles (located on the top of the wrist) and the wrist flexor muscles (located on the underside of the wrist) can both be affected by tendonitis.
- Knee: The quadriceps muscles (located on the front of the thigh) and the patellar tendon (located under the kneecap) are common sites for tendonitis in the knee.
- Ankle: The Achilles tendon (located at the back of the ankle) is a common site for tendonitis.
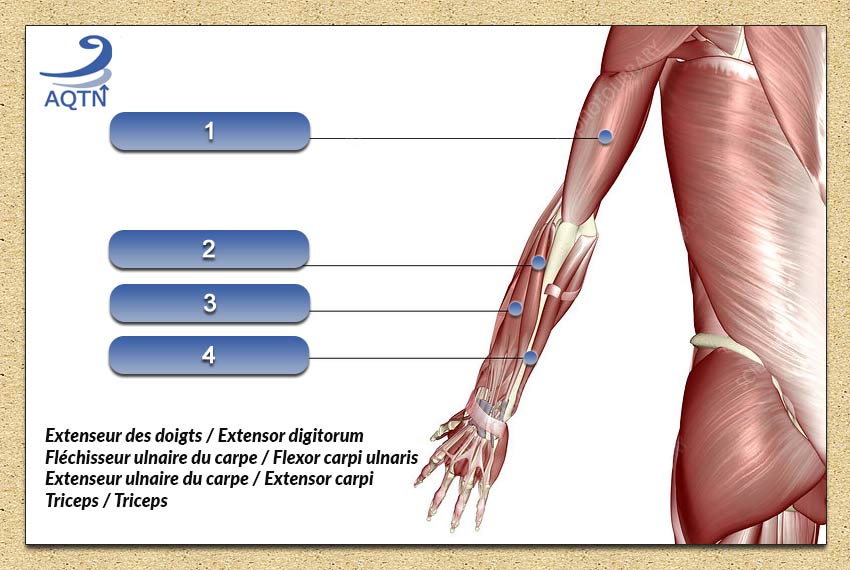
Tendonitis can occur in any muscle or tendon in the arm, but some of the most common muscles and tendons that are associated with tendonitis include:
- Rotator cuff muscles: The rotator cuff muscles (supraspinatus, infraspinatus, teres minor, and subscapularis) are located in the shoulder and are responsible for rotating and stabilizing the arm. Tendinitis in these muscles is common and is known as rotator cuff tendonitis.
- Biceps tendon: The biceps tendon is located at the front of the shoulder and attaches the biceps muscle to the shoulder blade. Biceps tendonitis is a common form of tendonitis that affects the biceps tendon.
- Triceps muscle: The triceps muscle is located at the back of the upper arm and is responsible for extending the elbow. Triceps tendonitis is a form of tendonitis that affects the triceps tendon.
- Forearm muscles: The forearm muscles (such as the wrist extensors and wrist flexors) are located in the lower arm and are responsible for moving the wrist and fingers. Tendinitis in the forearm muscles is common and is known as wrist tendonitis or hand tendonitis.
CARPEL TUNNEL
What is carpel tunnel
Carpal tunnel syndrome is a condition that occurs when the median nerve, which runs from the forearm into the hand, becomes compressed at the wrist. This can cause symptoms such as numbness, tingling, and weakness in the hand and fingers. There are several factors that can increase the risk of developing carpal tunnel syndrome, including:
- Repetitive hand and wrist movements: Jobs or hobbies that require repetitive hand and wrist movements, such as typing or knitting, can put added pressure on the median nerve and lead to carpal tunnel syndrome.
- Trauma or injury to the wrist: A wrist fracture or sprain can lead to swelling and inflammation, which can increase the risk of carpal tunnel syndrome.
- Rheumatoid arthritis: This autoimmune disorder can cause inflammation in the wrist and lead to carpal tunnel syndrome.
- Obesity: Excess weight can put added pressure on the median nerve and increase the risk of carpal tunnel syndrome.
- Pregnancy: Fluid retention during pregnancy can increase the risk of carpal tunnel syndrome.
- Thyroid problems: An overactive thyroid gland can cause swelling in the wrist, leading to carpal tunnel syndrome.
- Diabetes: People with diabetes are more prone to nerve damage and may be at an increased risk of developing carpal tunnel syndrome.
- Aging: The risk of carpal tunnel syndrome increases with age.
Massage therapy and carpel tunnel
Massage therapy can be an effective treatment for carpal tunnel syndrome as it can help to reduce muscle tension and inflammation in the wrist and hand. Massage therapy can also improve blood flow to the affected area and help to reduce pain and discomfort.
There are several massage techniques that can be used to treat carpal tunnel syndrome, including:
- Swedish massage: This type of massage uses long, flowing strokes to relax the muscles and improve circulation.
- Deep tissue massage: This type of massage uses deep, concentrated pressure to reach the deeper layers of muscle tissue. It can help to reduce muscle tension and inflammation.
- Trigger point therapy: This type of massage focuses on specific areas of the body where tension or “trigger points” are located. These points can cause pain and discomfort in other parts of the body, and trigger point therapy can help to release them.
- Acupressure: This type of massage uses finger pressure on specific points on the body to stimulate the flow of energy and improve circulation.
Clinical reasoning and treatment plan overview
A massage therapist would typically work with a client with carpal tunnel syndrome to develop a treatment plan that includes massage therapy as well as other treatments.
Such as stretching and strengthening exercises and splinting. The specific treatment plan will depend on the severity of the condition and the needs of the individual client.
Here are some common elements that may be included in a treatment plan for carpal tunnel syndrome:
- Massage therapy: Massage can help to reduce muscle tension and inflammation in the wrist and hand, as well as improve blood flow to the affected area. Massage therapists may use a variety of techniques, such as Swedish massage, deep tissue massage, trigger point therapy, and acupressure.
- Stretching and strengthening exercises: Stretching and strengthening exercises can help to improve flexibility and strength in the wrist and hand, which can help to alleviate symptoms of carpal tunnel syndrome.
- Splinting: Wearing a splint at night can help to keep the wrist in a neutral position and reduce pressure on the median nerve.
- Hot and cold therapy: Applying heat or cold to the affected area can help to reduce pain and inflammation.
- Medications: Over-the-counter pain medications, such as ibuprofen or acetaminophen, can help to reduce pain and inflammation. In more severe cases, a healthcare provider may prescribe stronger medications or corticosteroid injections.
- Surgery: In severe cases, surgery may be necessary to release the pressure on the median nerve.
- Rest! Stop or limit the actual repetitive motion causing the injury.
It’s important to note that treatment for carpal tunnel syndrome should be individualized to meet the needs of each person. A massage therapist would work closely with the client and possibly other healthcare providers to develop the most appropriate treatment plan.
Massage and pressure for carpel tunnel
The amount of pressure that is used during massage therapy on the wrist of a client with carpal tunnel syndrome should be determined on a case-by-case basis, taking into account the severity of the condition and the preferences of the client. In general, it is important to use a moderate amount of pressure that is comfortable for the client. If the client has a severe case of carpal tunnel syndrome or experiences pain when the wrist is touched, it may be best to avoid massaging the wrist and focus on other areas of the body.
The massage therapist should discuss the client’s symptoms and comfort level with them before beginning treatment. It may be helpful to use a lighter touch at first and gradually increase the pressure as the client becomes more comfortable. It is important to communicate with the client throughout the massage to ensure that the pressure is comfortable and to adjust the pressure as needed. The massage therapist should also watch for signs of discomfort or pain, and stop the massage if necessary.
Muscles related to carpel tunnel
The median nerve is responsible for providing sensation to the palm side of the thumb, index finger, middle finger, and half of the ring finger, as well as supplying motor function to some of the small muscles in the hand. The small muscles in the hand that are supplied by the median nerve include the thenar muscles, which are located in the palm of the hand, and the hypothenar muscles, which are located in the pinky finger side of the hand. These muscles are responsible for making the thumb and fingers move.
In addition to the median nerve, the carpal tunnel also contains the tendons of the flexor muscles in the forearm, which are responsible for bending the fingers and wrist. The flexor muscles include the flexor carpi radialis, the flexor carpi ulnaris, the palmaris longus, and the flexor digitorum superficialis. These muscles are located on the underside of the forearm and attach to the bones in the hand. The carpal tunnel also contains the tendons of the extensor muscles in the forearm, which are responsible for straightening the fingers and wrist. The extensor muscles include the extensor carpi radialis longus, the extensor carpi radialis brevis, the extensor carpi ulnaris, and the extensor digitorum. These muscles are located on the top side of the forearm and attach to the bones in the hand.
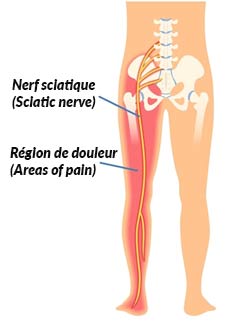
SCIATICA
About the sciatic nerve
The sciatic nerve is the largest nerve in the body and it runs from the lower back, through the buttocks, and down the legs. Sciatica is a term that refers to pain that is caused by irritation or compression of the sciatic nerve. Sciatica can be caused by a variety of things, such as a herniated disk in the lower spine, spinal stenosis (narrowing of the spinal canal), or a muscle spasm in the lower back. The pain associated with sciatica can range from mild to severe, and it can be a chronic (long-term) or acute (short-term) condition.
Massage therapy and sciatica
When a massage therapist is working with a client with sciatica, it is important to keep the following things in mind:
- Start with a gentle massage. Sciatica can be a painful condition, so it is important to start with gentle, soothing strokes to help the client relax.
- Avoid massaging directly over the sciatic nerve. The sciatic nerve runs down the back of the leg, so it is best to avoid massaging directly over it. Instead, focus on the surrounding muscles.
- Focus on the lower back and hips: Sciatica is often caused by problems in the lower back or hips, so it can be helpful to focus your massage on these areas. You can use techniques like effleurage (long, gliding strokes), petrissage (kneading or rolling), and tapotement (tapping or percussion) to loosen up tight muscles and encourage relaxation.
- Use long, gliding strokes. Long, gliding strokes can help to relax the muscles and reduce tension.
- Pay attention to the client’s comfort level. It is important to pay attention to the client’s comfort level and to stop the massage if they are experiencing pain.
- Use techniques to improve circulation. Techniques such as effleurage (stroking) and petrissage (kneading) can help to improve circulation and reduce muscle tension.
- Avoid trigger points: Trigger points are areas of muscle that are highly sensitive and can cause pain or discomfort when pressed. If you come across a trigger point while massaging your client, try to avoid applying direct pressure to it and instead work the surrounding muscles.
- Encourage stretching: Stretching can help to improve flexibility and reduce muscle tension, so you may want to encourage your client to stretch their lower back and hips before and after the massage. Be sure to give your client specific stretching instructions and caution them to stretch gently to avoid further irritation.
Massage pressure and sciatica
When massaging a client with sciatica, it is important to be mindful of the amount of pressure that you use. Applying too much pressure can cause further irritation or pain to the sciatic nerve and surrounding muscles, while not applying enough pressure may not be effective in releasing tension or discomfort.
A general rule of thumb is to start with light to moderate pressure and gradually increase the pressure as needed and as tolerated by the client. You can also ask your client for feedback during the massage to gauge their comfort level and adjust the pressure accordingly.
It can be helpful to use a variety of techniques and pressures during the massage to find the right balance of effectiveness and comfort. For example, you could begin with long, gentle strokes to warm up the muscles and stimulate blood flow, and then gradually increase the pressure as you work on specific areas of tension. You could also use techniques like petrissage (kneading or rolling) or tapotement (tapping or percussion) to apply deeper pressure to specific muscle groups.
Remember to always listen to your client’s feedback and be prepared to adjust your technique as needed to ensure that you are providing a comfortable and effective massage. The amount of pressure that you should use when massaging a client with sciatica will depend on the individual’s pain level and tolerance. In general, it is important to start with a lighter touch and gradually increase the pressure as you go, taking care to listen to your client’s feedback and stop if they experience any discomfort.
If your client is experiencing severe pain, it may be best to avoid deep tissue techniques and instead use a more gentle approach such as Swedish massage. Swedish massage involves long, flowing strokes that are designed to relax the muscles and improve circulation. You can use light to moderate pressure when performing Swedish massage techniques, taking care to avoid pressing too hard on any sensitive areas.
If your client is able to tolerate more pressure and is interested in deep tissue work, you can use techniques such as trigger point therapy or myofascial release to address specific areas of muscle tension. When performing deep tissue techniques, it is important to use a firm, steady pressure and to communicate with your client about the amount of pressure they are comfortable with.
Muscles involved in sciatica
The muscles that are most commonly involved in sciatica are those in the lower back and hips. These muscles include:
- The piriformis muscle: This muscle is located in the buttocks and it helps to rotate the leg outward.
- The gluteus maximus muscle: This muscle is the largest muscle in the buttocks and it helps to extend the hip and rotate the leg outward.
- The erector spinae muscles: These muscles are a group of long, thin muscles that run along the spine and help to extend the back and maintain good posture.
- The quadratus lumborum muscle: This muscle is located in the lower back and it helps to flex the spine and maintain good posture.
- The hip flexor muscles: These muscles, which include the iliopsoas, rectus femoris, and sartorius muscles, are located in the front of the hip and they help to flex the hip joint.
Clinical judgement as a therapist
There are a few key considerations that a massage therapist should take into account when working with a client who has low-level pain due to sciatica:
- Assess the client’s pain level: It is important to ask the client about the intensity and location of their pain, as well as any other symptoms they may be experiencing. This will help you to understand the client’s condition and determine the best course of treatment.
- Identify the underlying cause of the pain: Sciatica can be caused by a variety of different factors, such as a herniated disk, spinal stenosis, or muscle spasms in the lower back. Understanding the specific cause of the client’s pain can help you to tailor your treatment approach and focus on the most relevant muscle groups.
- Consider the client’s medical history: Be sure to ask the client about any medical conditions or injuries they may have, as well as any medications they are taking. This information can help you to anticipate any potential contraindications or precautions that may need to be taken during the massage.
- Use a gentle touch: With low-level pain, it is generally safe to use a gentle touch and a more relaxing massage technique, such as Swedish massage. Avoid using deep tissue techniques or applying too much pressure, as this may cause discomfort or further irritation.
- Encourage the client to communicate: It is important to encourage the client to speak up if they experience any discomfort or pain during the massage. This will allow you to adjust your technique and ensure that you are providing the most comfortable and effective treatment possible.
By taking these considerations into account, you can help to ensure that you are providing the best possible care for your client with sciatica and helping them to manage their pain and improve their quality of life.
LOWER BACK PAIN
Common causes of lower back pain
There are many different things that can cause lower back pain, including:
- Muscular strain or sprain: Overuse or injury to the muscles, ligaments, or tendons in the lower back can cause pain and stiffness.
- Herniated disk: A herniated disk occurs when the soft, jelly-like material inside the disk bulges out through a tear in the outer layer. This can put pressure on the nerves in the spine and cause lower back pain.
- Spinal stenosis: This occurs when the spaces in the spine become narrowed, which can put pressure on the nerves and cause lower back pain.
- Osteoarthritis: This is a type of degenerative joint disease that can cause pain and stiffness in the lower back.
- Sciatica: This is a term that refers to pain that is caused by irritation or compression of the sciatic nerve, which runs from the lower back, through the buttocks, and down the legs.
- Scoliosis: This is a condition in which the spine is curved to one side, which can cause lower back pain.
- Poor posture: Maintaining poor posture for extended periods of time can lead to muscle strain and lower back pain.
There are many other possible causes of lower back pain
Massage and pressure for lower back pain
The amount of pressure that a massage therapist should use for lower back pain will depend on the individual’s pain level and tolerance. In general, it is important to start with a lighter touch and gradually increase the pressure as you go, taking care to listen to the client’s feedback and stop if they experience any discomfort.
If the client is experiencing severe pain, it may be best to avoid deep tissue techniques and instead use a more gentle approach such as Swedish massage. You can use light to moderate pressure when performing Swedish massage techniques, taking care to avoid pressing too hard on any sensitive areas.
If the client is able to tolerate more pressure and is interested in deep tissue work, you can use techniques such as trigger point therapy or myofascial release to address specific areas of muscle tension. When performing deep tissue techniques, it is important to use a firm, steady pressure and to communicate with the client about the amount of pressure they are comfortable with. Remember to listen to the client’s feedback and stop if they experience any discomfort.
It’s important to remember that every person is different and may respond differently to massage. It’s always a good idea to communicate with the client and ask for feedback to ensure that you are providing the most comfortable and effective treatment possible.
Muscles involved in lower back pain
Lower back pain can be caused by a variety of different factors, and the specific muscles that are involved will depend on the cause of the pain. Some common muscle groups that can contribute to lower back pain include:
- The multifidus: This is a small muscle that runs the length of the spine and helps to support the spine and maintain proper posture.
- The erector spinae: This group of muscles runs along the sides of the spine and is responsible for helping us to maintain an upright position.
- The quadratus lumborum: This muscle is located on the sides of the lower back and helps to support the spine and move the hips.
- The gluteal muscles: These muscles, which include the gluteus maximus, gluteus medius, and gluteus minimus, are located in the buttocks and are responsible for supporting the body’s weight and helping us to move our legs and hips.
- The hip flexors: These muscles, which include the iliopsoas and the rectus femoris, are located in the front of the hips and are responsible for flexing the hip joint.
Tips for working with a client with lower back pain
When assessing lower back pain, it is important for a massage therapist to consider a number of factors in order to develop an effective treatment plan. Here are a few key considerations to keep in mind:
- Assess the client’s pain level: It is important to ask the client about the intensity and location of their pain, as well as any other symptoms they may be experiencing. This will help you to understand the client’s condition and determine the best course of treatment.
- Identify the underlying cause of the pain: Lower back pain can be caused by a variety of different factors, such as muscle strain, a herniated disk, spinal stenosis, or osteoarthritis. Understanding the specific cause of the client’s pain can help you to tailor your treatment approach and focus on the most relevant muscle groups.
- Consider the client’s medical history: Be sure to ask the client about any medical conditions or injuries they may have, as well as any medications they are taking. This information can help you to anticipate any potential contraindications or precautions that may need to be taken during the massage.
- Assess the client’s posture: Poor posture can contribute to lower back pain, so it is important to assess the client’s posture and identify any areas of muscle tension or imbalance.
- Consider the client’s lifestyle: The client’s daily activities and occupation may also be contributing to their lower back pain, so it can be helpful to ask about their work and leisure habits.
By taking these considerations into account, you can develop a treatment plan that is tailored to the specific needs of the client and is most likely to help alleviate their lower back pain and improve their quality of life.
INJURED PECTORALS
About pectorals
The pectoral muscles, also known as the pectorals or pecs, are a group of muscles located in the chest. They are responsible for moving the arms and shoulders and are important for activities such as lifting, pushing, and pulling. The pectoral muscles are made up of two main muscles: the pectoralis major and the pectoralis minor. The pectoralis major is the larger of the two muscles and is responsible for moving the arm across the body (adduction) and rotating it inward (internal rotation). The pectoralis minor is a smaller muscle located underneath the pectoralis major and is responsible for moving the shoulder blade (scapula) downward and forward. The pectoral muscles are important for maintaining good posture and are often trained in strength and conditioning exercises. They can be exercised using a variety of different exercises, such as push-ups, chest presses, and chest flies.
The pectoral muscles are connected to a number of bones in the body, including:
- The sternum: The pectoral muscles are connected to the sternum, or breastbone, which is a long, flat bone located in the center of the chest.
- The clavicle: The pectoral muscles are also connected to the clavicle, or collarbone, which is a long, thin bone that runs between the sternum and the shoulder blade (scapula).
- The scapula: The pectoral muscles are connected to the scapula, or shoulder blade, which is a triangular-shaped bone located on the back of the shoulder.
- The humerus: The pectoral muscles are connected to the humerus, which is the bone in the upper arm.
By connecting to these bones, the pectoral muscles are able to move the arms and shoulders and play a role in activities such as lifting, pushing, and pulling.
Massage therapy and the pectorals
Massage therapy can be helpful for relieving tension and improving flexibility in the pectoral muscles. Some specific techniques that a massage therapist might use to target the pectoral muscles include:
- Petrissage: This technique involves kneading or rolling the muscles between the thumb and fingers or with the palm of the hand.
- Effleurage: This technique involves long, flowing strokes that are designed to relax the muscles and improve circulation.
- Cross-fiber friction: This technique involves using small circular motions to apply pressure across the fibers of the muscle.
- Trigger point therapy: This technique involves applying pressure to specific points within the muscle that are known as trigger points, which can cause pain and discomfort when they are tight or overactive.
- Myofascial release: This technique involves applying sustained pressure to the fascia (a thin layer of connective tissue surrounding the muscles) to help release tension and improve flexibility.
By incorporating these techniques into a massage session, a therapist can help to alleviate muscle tension and improve mobility in the pectoral muscles. As with any massage treatment, it is important to communicate with the client about their comfort level and to adjust the technique as needed.
Massage pressure
When working with a client who has tension in their pectoral muscles, it is important for a massage therapist to consider the following:
- The client’s pain level: It is important to ask the client about the intensity of their muscle tension and any associated pain, as well as their pain tolerance. This will help you to determine the appropriate amount of pressure to use during the massage.
- The client’s body type: The thickness and density of the pectoral muscles can vary from person to person, so it is important to consider the client’s body type when determining the appropriate amount of pressure to use.
- The client’s preference: Some clients may prefer a more relaxing massage with lighter pressure, while others may prefer a deeper, more therapeutic massage. It is important to ask the client about their preference and to adjust the pressure accordingly.
- The client’s age and physical condition: Older clients or those with certain medical conditions may have a lower tolerance for pressure, so it may be necessary to use a lighter touch with these clients.
- Assess the client’s posture: Poor posture can contribute to tension in the pectoral muscles, so it is important to assess the client’s posture and identify any areas of muscle tension or imbalance.
- Consider the client’s lifestyle: The client’s daily activities and occupation may also be contributing to their muscle tension, so it can be helpful to ask about their work and leisure habits.
- Stretches, it is often important to start the process of opening of the pectorals.
HAMSTRING AND IT BAND INJURIES
Common causes
There are several common causes of hamstring and IT band injuries, including:
- Overuse: Repeatedly using the hamstrings and IT band without giving them sufficient rest can lead to muscle strain or inflammation.
- Poor stretching habits: Failing to properly stretch before exercise or physical activity can increase the risk of injury to the hamstrings and IT band.
- Weakness in the glutes: Weak gluteal muscles (located in the buttocks) can lead to an imbalance in muscle strength, increasing the risk of injury to the hamstrings and IT band.
- Poor footwear: Wearing shoes that do not provide adequate support or cushioning can increase the risk of injury to the hamstrings and IT band.
- Sudden changes in activity level: Rapidly increasing the intensity or duration of physical activity without adequate preparation can lead to muscle strain or inflammation.
- Poor technique: Using improper technique when exercising or engaging in physical activity can increase the risk of injury to the hamstrings and IT band.
Muscles involved
The iliotibial (IT) band is a thick band of fascia that runs along the outside of the leg, from the pelvis to the tibia (shin bone). It attaches to several muscles, including the gluteus maximus, tensor fasciae latae, and the biceps femoris (a muscle in the hamstring group).
The hamstrings are a group of three muscles located at the back of the thigh. They include the:
- Biceps femoris: This muscle has two heads, a long head and a short head. The long head originates from the ischial tuberosity (sit bone) and the short head originates from the linea aspera (a ridge on the femur). Both heads attach to the head of the fibula (a bone in the lower leg).
- Semitendinosus: This muscle originates from the ischial tuberosity and inserts into the upper part of the tibia.
- Semimembranosus: This muscle originates from the ischial tuberosity and inserts into the medial condyle of the tibia (a bony prominence on the inner part of the tibia).
Clinical reasoning for IT band
As a massage therapist, it’s important to start with a light touch when working on injured hamstrings and gradually increase the pressure as tolerated. It’s also important to listen to the individual’s feedback and adjust the pressure accordingly. If the individual experiences sharp or shooting pain, it’s important to reduce the pressure and notify the therapist.
It’s also important to keep in mind that massage therapy should not cause pain. If the individual is experiencing pain during the massage, it’s important to communicate this to the therapist and adjust the technique or pressure as needed. It’s also important to consider the severity of the injury when determining the appropriate level of pressure.
For more severe injuries, it may be necessary to use a lighter touch initially and gradually increase the pressure as the individual’s pain and discomfort improve. One should always be mindful of the individual’s comfort level and feedback.
Tous ces muscles travaillent ensemble pour fléchir la hanche, étendre le genou et faire tourner la jambe vers l’intérieur. Ils aident également à stabiliser le bassin et à maintenir l’équilibre lorsqu’on se tient sur une jambe.
Massage therapy and the IT band
There are several massage therapy techniques that can be effective for addressing issues with the IT band and/or hamstrings. Some options include:
Les ischiojambiers sont un groupe de trois muscles situés à l’arrière de la cuisse. Ils comprennent les :
- Friction Massage: This technique involves applying deep pressure to the IT band or hamstrings using the fingertips or knuckles. The therapist may use circular or back and forth motions to apply the pressure.
- Cross-Fiber Friction: This technique involves using the fingertips or knuckles to apply pressure across the fibers of the muscle. This can help to break up scar tissue and improve flexibility.
- Myofascial Release: This technique involves applying sustained pressure to the IT band or hamstrings using the palms of the hands or a foam roll. The therapist may use a rocking motion to help release tension in the muscle.
- Trigger Point Therapy: This technique involves applying pressure to specific points within the muscle known as “trigger points,” which can cause pain and tightness.
MASSAGE THERAPY AND ANKLE STRAIN
Massage therapy can be an effective treatment option for individuals with ankle strain. Massage can help to reduce inflammation and swelling, improve circulation, and reduce muscle tension. It can also help to improve range of motion and flexibility, which can be beneficial during the recovery process.
Massage pressure for an ankle strain
The appropriate level of pressure to use when massaging a client with ankle strain will depend on the severity of the injury and the individual’s pain tolerance. In general, it’s important to start with a light touch and gradually increase the pressure as tolerated. It’s important to listen to the individual’s feedback and adjust the pressure accordingly. If the individual experiences sharp or shooting pain, it’s important to reduce the pressure and notify the therapist. It’s also important to keep in mind that massage therapy should not cause pain. If the individual is experiencing pain during the massage, it’s important to communicate this to the therapist and adjust the technique or pressure as needed.
It’s also important to consider the stage of recovery when determining the appropriate level of pressure. For more severe injuries or early in the recovery process, it may be necessary to use a lighter touch initially and gradually increase the pressure as the individual’s pain and discomfort improve. In general, it’s important to use a gentle touch and gradually increase the pressure as tolerated, while always being mindful of the individual’s comfort level and feedback.
Muscles related to the ankle
The ankle joint is formed by the tibia (shin bone) and the fibula (a bone in the lower leg) and is supported by a network of muscles, tendons, and ligaments. Some of the muscles and tendons that are connected to the ankle include:
- Tibialis anterior: This muscle originates from the upper two-thirds of the tibia and inserts into the base of the first metatarsal bone (a bone in the foot). It is responsible for flexing the ankle and toes and for turning the foot inward.
- Peroneus longus: This muscle originates from the head of the fibula and the upper two-thirds of the fibula and inserts into the base of the first metatarsal bone. It is responsible for everting (turning outward) the foot and ankle.
- Peroneus brevis: This muscle originates from the lower two-thirds of the fibula and inserts into the base of the fifth metatarsal bone (a bone in the foot). It is responsible for everting the foot and ankle.
- Gastrocnemius: This muscle originates from the posterior (back) of the femur (thigh bone) and inserts into the calcaneus (heel bone). It is responsible for plantar flexing (pointing) the foot and ankle.
- Soleus: This muscle originates from the posterior of the tibia and fibula and inserts into the calcaneus. It is responsible for plantar flexing the foot and ankle.
- Achilles tendon: This tendon connects the gastrocnemius and soleus muscles to the calcaneus and is responsible for plantar flexing the foot and ankle.
Clinical reasoning and massage therapy for ankle strain
These muscles and tendons work together to allow for movement and stability in the ankle joint.
- It may be necessary to use a gentler touch and focus on techniques that can help to reduce inflammation and pain, such as myofascial release or trigger point therapy. As the injury improves, the therapist can gradually increase the intensity of the massage and incorporate techniques that can help to improve flexibility and range of motion.
- Stage of recovery: It’s important to consider the stage of recovery when developing a treatment plan. Early in the recovery process, the focus may be on reducing inflammation and pain and promoting healing. As the injury improves, the therapist can focus on techniques that can help to improve flexibility and range of motion.
- Presence of other injuries or conditions: It’s important to consider any other injuries or conditions that the client may have, as these may impact the treatment approach. For example, if the client has diabetes, the therapist may need to use a gentler touch and be mindful of the risk of nerve damage.
- Client preferences: It’s important to involve the client in the decision-making process and consider their treatment goals and preferences. The therapist should work with the client to determine the most appropriate treatment approach and adjust the treatment plan as needed.
SUMMARY OF SOME OF THE MUSCLES REFERENCED IN THIS ARTICLE
Neck muscles
- Sternocleidomastoid
- Scalenes
- Splenius
- Levator scapula
- Trapezius
Tendonitis
- Shoulder: rotator cuff & biceps
- Wrist (forearm): extensor and flexor muscles
- Thenar and hypothenar muscles (moves fingers & thumbs).
Rotator cuff
- Supraspinatus
- Infraspinatus
- Teres minor
- Subscapularis
Sciatica
- Piriformis
- Gluteus maximus
- Erector spinae
- QL
- Hip flexors: iliacus, psoas, pectineus, rectus femoris, sartorius.
Lower back pain
- Multifidus
- Erector spinae
- QL
- Glutes
- Hip flexors (5): as above.
Ankle
- Tibialis anterior
- Peroneus longus
- Peroneus brevis
- Gastrocnemius
- Soleus
IT band / Hamstrings
- IT band (attaches to gluteus maximus, tensor fascialatae, biceps femoris)
- Biceps femoris
- Semitendinosus
- Semimembranosus

Pectorals
- Pectoral muscles
Arm flexer muscles
- Flexor carpi ulnaris
- Flexor carpi radialis
- Palmarus longus
- Flexor digitorum superficialis
